Cara August, Trinity Communications
“When was the last time you thought — who is white?” asked Jen’nan Read, chair and professor in the department of Sociology, whose newly published study in the “Journal of Immigrant and Minority Health” examines the data integrity of using the “white” racial category as a benchmark when comparing racial and ethnic health disparities.
“It’s the group to which all other groups in the U.S. are compared,” Read said.
With the release of her new study, Read is working to fill a gap in the literature — becoming the first researcher to look at both physical and mental health outcomes among all U.S. whites, both foreign- and native-born.

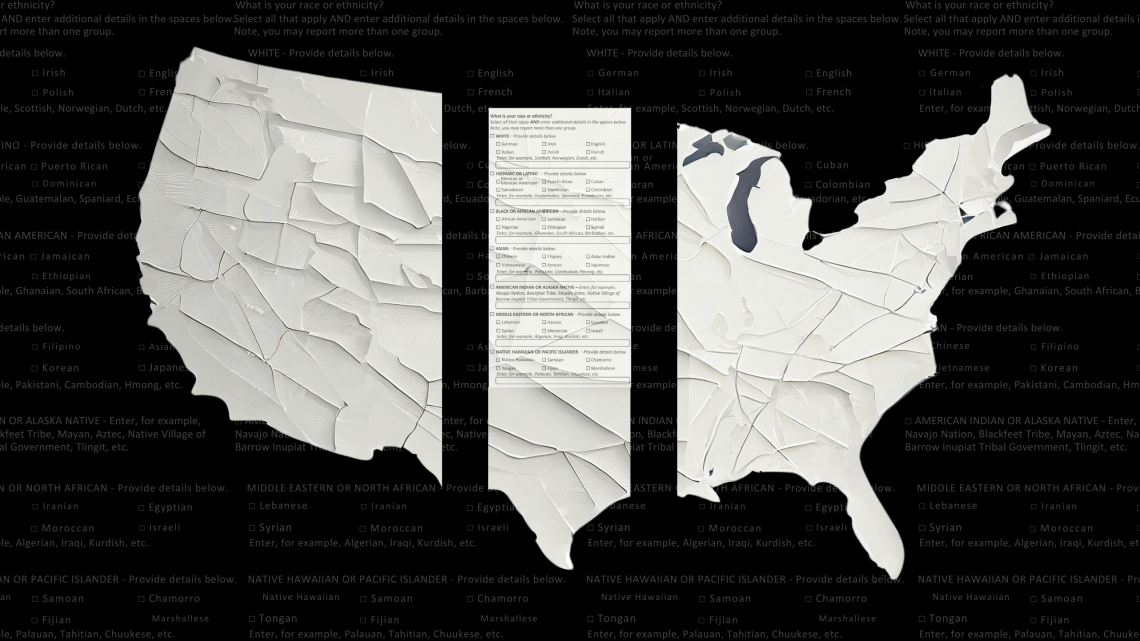
But who is white? According to the U.S. Census, any person — immigrant or U.S.-born — who traces their ancestry to Europe, the Middle East or North Africa (MENA) is defined as white. Together, they make-up the white category used for health data reporting and all other types of racial data analysis in the United States.
But within that white racial category are diverse ethnic subgroups and many people of MENA descent who do not feel authentically represented by the white racial designation. For Read, and many other researchers, the grouping is problematic because subgroups of a larger ‘model’ demographic are often disregarded in health reporting.
For example, Read — a Carnegie scholar and expert on social determinants of health disparities among Arab and Muslim populations — found that every time she needed to pull health data for Arab Americans, she’d have to peel it out of from within the white category.
“When lumped together in this broad white category, health disparities within a subgroup population can be easily overlooked,” she said.
But finding health data on whites also proved a challenge for Read, who says that surprisingly little research exists on ethnic diversity in health among whites.
“We know relatively little about the health of groups who are classified within the white population, especially if you consider how much we know about groups who are classified within the Hispanic, Asian and Black populations,” Read said. “If we really care about equity, we need to care about who is classified as white because when we talk about health, it's typically in reference to white health.”
Read’s study could have a significant impact on illuminating the importance of studies that separate and examine ethnic subgroups of racial categories, such as Arab Americans and eastern Europeans.
The federal government established standards on racial classification in 1977, in the wake of the Civil Rights Movement, because they needed consistent and comparable data on race and ethnicity to enforce Civil Rights laws and ensure the equitable distribution of resources.
At the time, western European whites comprised over 70 percent of the total U.S. population and 60 percent of the foreign-born white population. Today, those numbers have dropped to roughly one-third each, with Middle Eastern and eastern European immigrant populations — both classified as white — having grown to comprise over one-half of the foreign-born white population at 53 percent.
Based on nationally representative survey data, Read analyzed three self-reported health conditions, including depression, anxiety and self-rated health, and three diagnosed health conditions, including high blood pressure, diabetes and chronic obstructive pulmonary disease (COPD).
The results concluded that foreign-born whites had significantly lower prevalence of each health outcome relative to U.S.-born whites — a result known in the literature known as the “immigrant health advantage.” However, the data suggest that the advantage is smaller for foreign-born whites than it is for other racial or ethnic subgroups, indicating important variations in health among whites that is missed in studies that focus on U.S.-born whites, alone.
With 17 percent of immigrants in the U.S. classified as white — that’s one in six of the U.S. immigrant population — Read’s study asserts that scholars must continue to monitor the health of white immigrants, who are projected to grow to 20 percent of the US immigrant population by 2060.
Read’s hope for the research is that it opens a door to understanding the ethnic diversity that exists within the white category, leading to greater interest and inquiry into how and why the group is so often used as a health benchmark.
“White is the category that researchers have used for decades to benchmark everything, from health disparities to population growth to wealth inequality, with little interrogation or questioning,” Read said. “Not understanding diversity within broad racial categories hurts everybody,” she said. “It’s time we do better.”